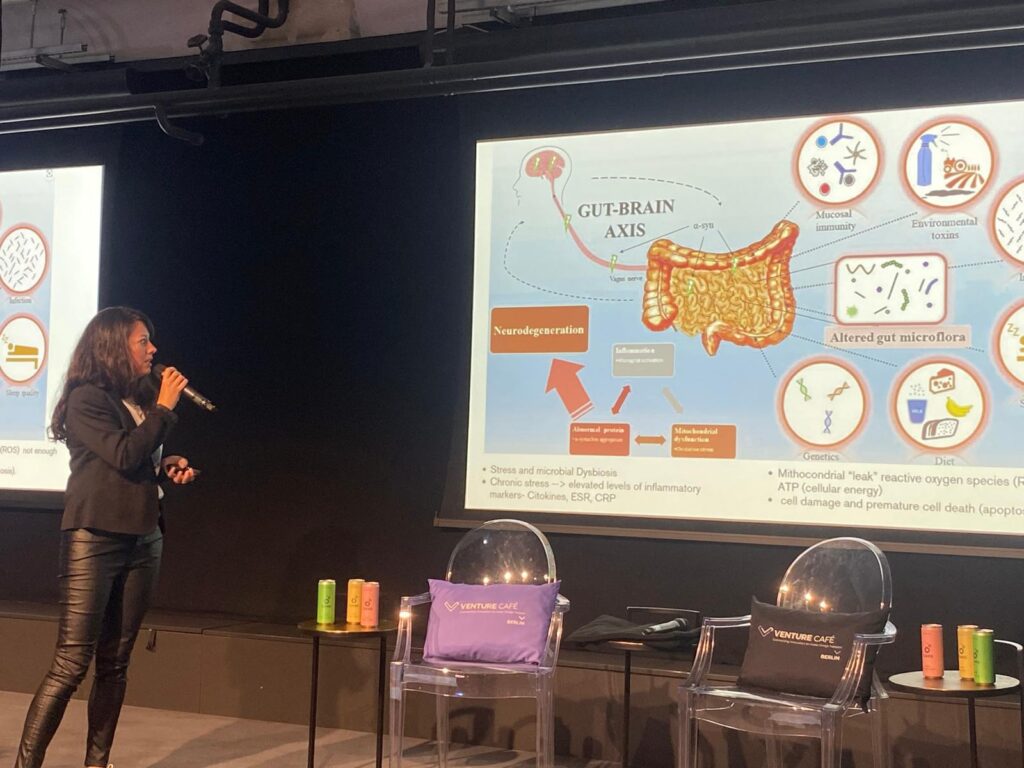
Scientists often refer to the gut as our “second brain.” This isn’t just a metaphor, it has its own nervous system, communicates directly with the brain, and deeply influences how we think, feel, and perform. The gut-brain axis (GBA) is a complex two-way communication network linking the gastrointestinal system with the central nervous system through neural pathways, hormones, and immune signaling. At the center of this connection is the gut microbiome, a vibrant ecosystem of trillions of microorganisms that play a fundamental role in supporting brain and body health.
When this communication system functions smoothly, we experience mental clarity, strong immunity, better digestion, and emotional stability. When it is disrupted, inflammation can increase, mood can decline, and the risk of chronic diseases grows.
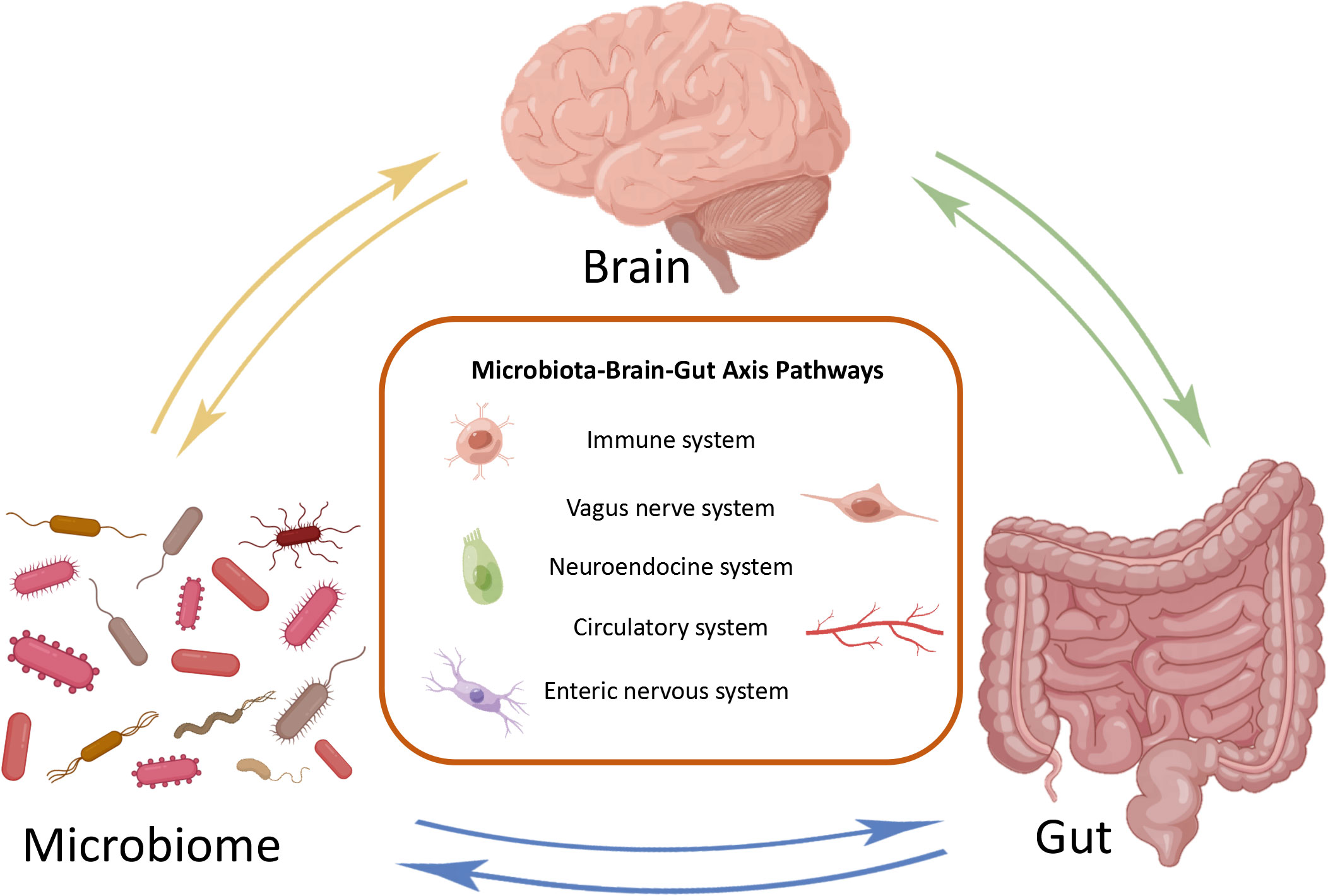
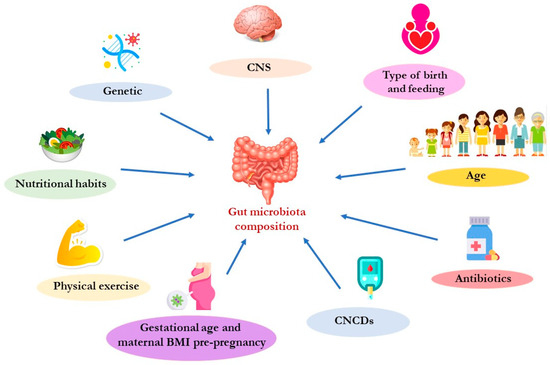
The gut-brain axis is much more than a communication route between the digestive system and the brain, it is a central regulator of both immune and endocrine function. Over 70% of the immune system resides in the gut, meaning that the microbiome continuously interacts with immune cells, training them to distinguish between what is safe and what is harmful. When the gut is in balance, beneficial bacteria help maintain a strong intestinal barrier, reducing systemic inflammation and protecting the brain from inflammatory signals. However, when dysbiosis occurs, (often driven by stress, infections, poor diet, or environmental toxins) the immune system can become overactive, contributing to chronic inflammation linked to anxiety, depression, and autoimmune disorders.
At the same time, the gut and brain communicate through a delicate hormonal network. Gut bacteria influence essential neurotransmitters and hormones, including serotonin (90% of which is produced in the gut), dopamine, melatonin, and cortisol. These chemical messengers help regulate sleep, mood, motivation, and how we react to stress. If the microbiome becomes imbalanced, these hormones can shift toward patterns associated with stress sensitivity, mood disturbances, and metabolic issues.
This combined impact on immunity and hormonal regulation explains why disturbances in the gut-brain axis are increasingly recognized in chronic inflammatory and endocrine-related conditions, from depression and ADHD to autoimmune diseases, chronic fatigue, thyroid dysfunction, and irritable bowel syndrome (IBS).
Growing evidence suggests that dysbiosis in the gut may worsen conditions like anxiety, depression, ADHD, autism and cognitive decline. Imbalances in bacterial strains can alter neurotransmitter production and increase neuroinflammation, which may intensify emotional reactivity and reduce stress tolerance.
Psychobiotics, specific strains of probiotics that support neurotransmitter production, have shown promising results in improving emotional regulation and reducing anxiety. Nutritional strategies, mindfulness-based practices, and movement therapies that activate the parasympathetic nervous system also contribute to strengthening gut-brain communication. When the microbiome is supported, individuals often experience a clearer mind, improved focus, and better emotional stability.
This is particularly important for neurodivergent individuals who frequently experience sensory stress, digestive issues, and autonomic nervous system dysregulation. Holistic approaches that support both gut health and nervous system activation can be transformative for this population.
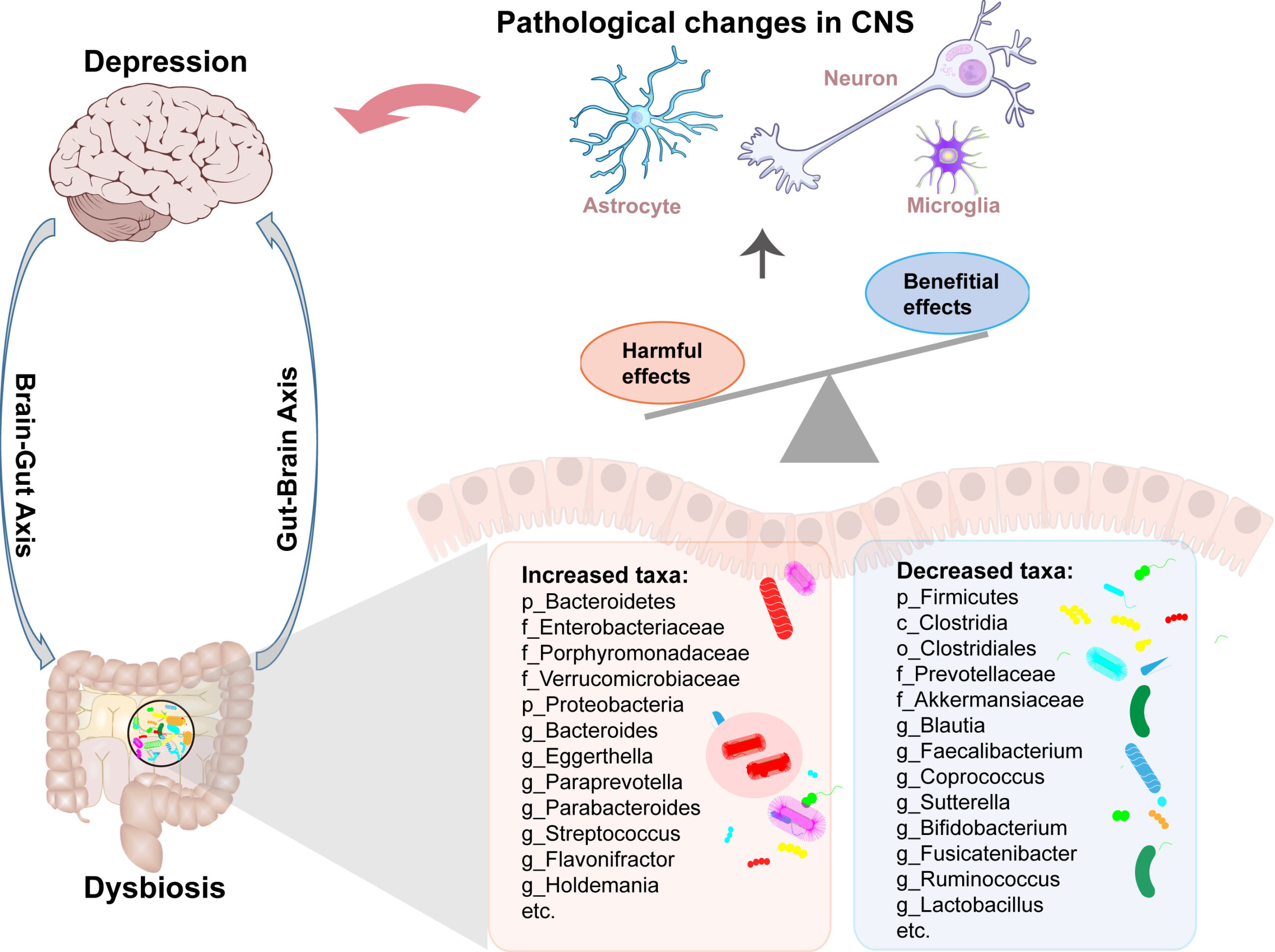
Disruptions in gut-brain communication are increasingly linked to non-communicable diseases such as metabolic syndrome, cardiovascular disease, type 2 diabetes, neurodegenerative disorders, and autoimmune diseases. Chronic low-grade inflammation, driven by dysregulated microbiome signaling, can accelerate aging and weaken the body’s metabolic and neurological resilience.
Understanding the gut-brain axis helps us identify risks earlier and offers new therapeutic possibilities that don’t rely solely on medications. This includes lifestyle interventions aimed at restoring equilibrium through nutrition, stress care, movement, and nervous system balance.
Your gut-brain axis thrives when your nervous system is supported and that is exactly what we help you achieve at Corner of Movement. Through Psychoneuroimmunology (PNI) health coaching, we guide individuals to restore balance and reduce neuro-immune stress using science-based lifestyle strategies. Our Healthy Productivity programs for organizations empower teams to prevent burnout, improve performance, and build emotionally healthy workplaces that protect long-term health. And with Qi Gong, we integrate mindful movement and vagus-nerve activation to enhance resilience, mobility, and emotional regulation.
Whether you’re an individual seeking deeper healing or a company aiming to protect your people, we’re here to support you with the tools your body and brain need to thrive.
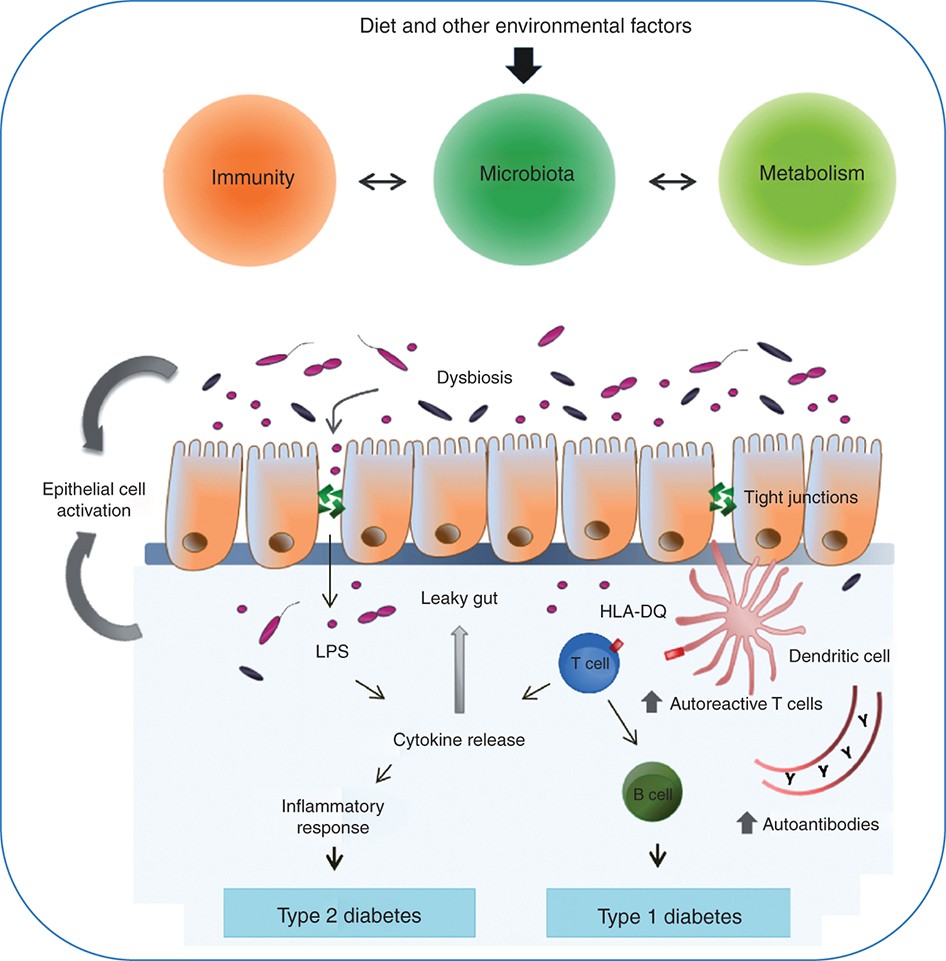
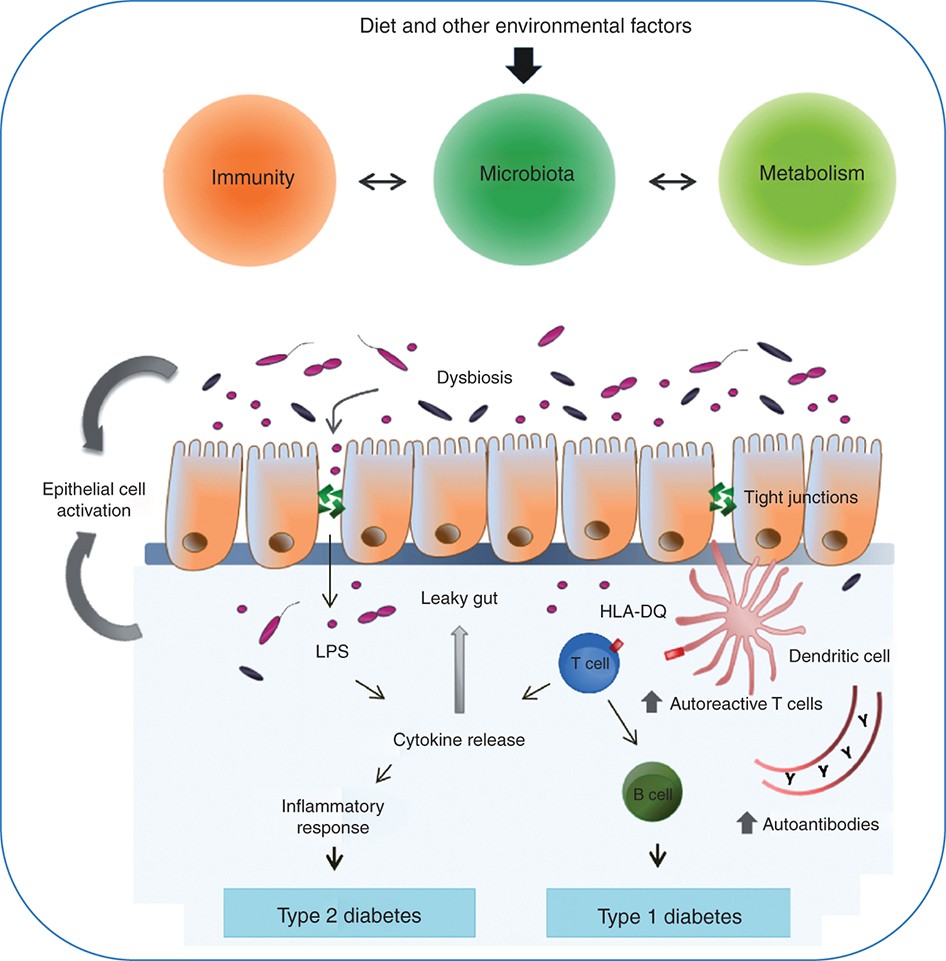
Autoimmune diseases are not sudden events. They often evolve through a sustained interplay of underlying factors: chronic stress, a disrupted microbiome, increased intestinal permeability, immune dysregulation, and persistent inflammation. Visualise the diagram you have: dysbiosis and stress feed into a compromised intestinal barrier (often described as “leaky gut”), which permits antigenic material to escape into the bloodstream, spurring immune activation, systemic inflammation, and ultimately autoimmune reactions.
Modern life places relentless demands on our nervous system. Prolonged stress alters gut motility, reduces beneficial microbial diversity and shifts the microbiome toward pro-inflammatory species. This dysbiosis weakens the gut’s microbial ecosystem—its first line of immune regulation—and primes the body for further dysfunction. Research now shows that altered gut microbial populations fuel autoimmune processes in conditions such as type 1 diabetes, multiple sclerosis and rheumatoid arthritis. PMC+1
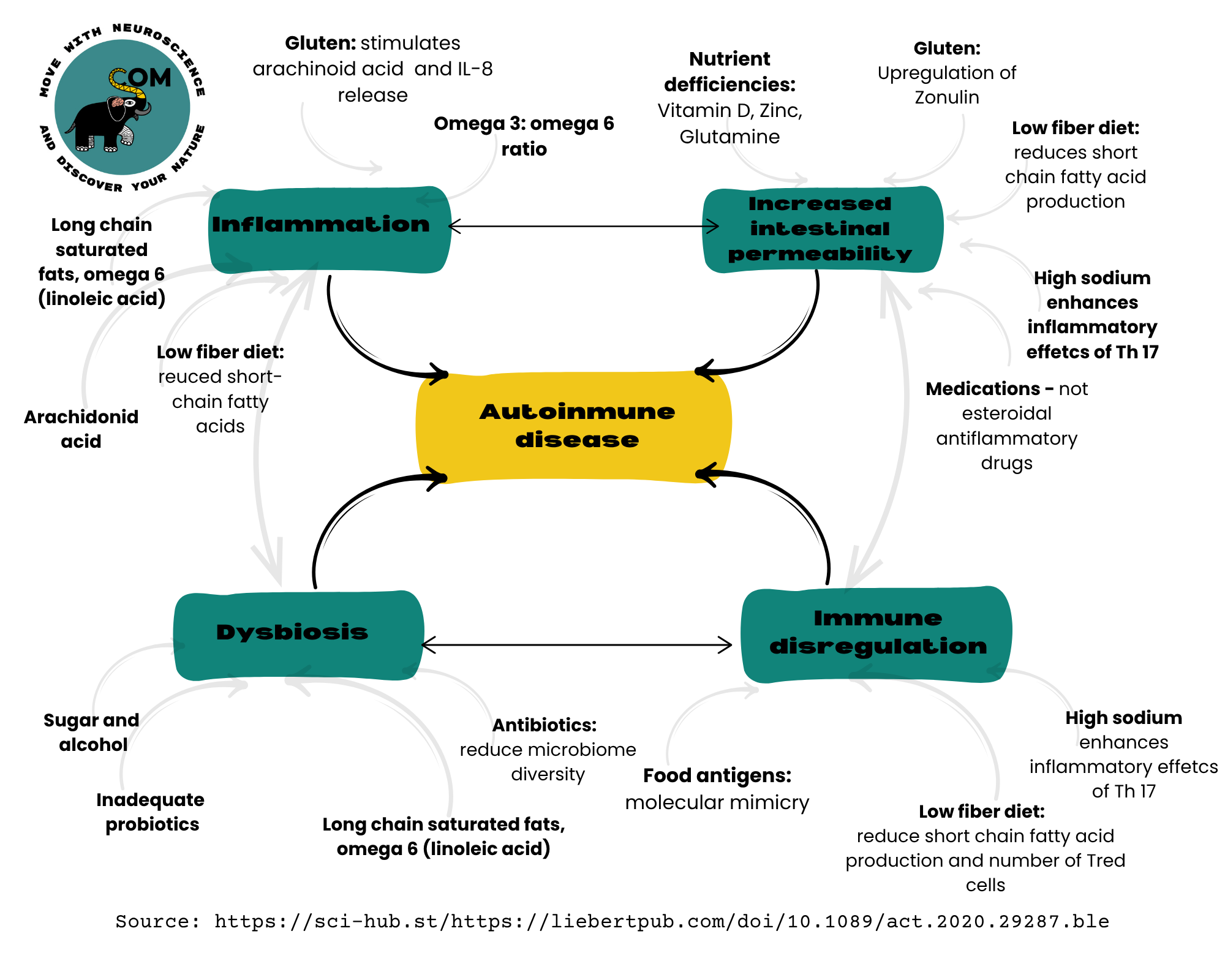
As dysbiosis deepens, the intestinal epithelium (our barrier to the outside world) begins to leak. Tight-junction proteins such as occludin and zonulin become disturbed, allowing microbial fragments, toxins and undigested proteins to pass into the circulation. Elevated serum markers of zonulin/occludin now correlate with autoantibody levels and autoimmune diagnoses. PubMed+1 Once the barrier is breached, the immune system is forced to respond—not only to pathogens but to mis-placed antigens, setting the stage for misdirected immune attacks on self-tissues.
When the gut barrier fails, immune cells in the lamina propria are exposed to previously contained stimuli; this triggers activation of dendritic cells, T cells, and B cells, shifting immune regulation away from tolerance and toward persistent activation. The outcome is an immune system that reacts more readily to self-antigens, driving both local and systemic inflammation. Evidence shows that increased permeability is present in brains, endocrine glands, joints and skin of people with autoimmune disorders. PMC+1
Chronic low-grade inflammation is the common thread linking stress, dysbiosis, leaky gut and autoimmunity. Microbial products crossing the gut barrier stimulate inflammatory cytokines such as IL-8, TNF-α and IL-17, and this inflammatory tone supports the perpetuation of autoimmune disease. Simultaneously, nutritional deficiencies (e.g., in vitamin D, zinc, glutamine), high-sugar/low-fiber diets, and lifestyle habits add fuel to this fire, amplifying intestinal permeability and immune activation. PubMed+1
What begins as dysbiosis-induced barrier compromise can lead to immune activation which further disrupts microbial homeostasis and increases permeability—creating a vicious cycle. As shown in your image, the loop of dysbiosis → increased intestinal permeability → immune dysregulation → inflammation sustains and heightens autoimmune risk. Breaking this loop is key to prevention and healing.
The gut-brain axis is a dynamic communication network that responds to how we eat, move, breathe, and handle stress. When we nurture our digestive system and regulate our nervous system, everything improves, from immune strength and hormone balance to productivity, emotional well-being, and personal vitality.
In the landscape of autoimmune disease, stress is the spark, dysbiosis is the tinder, leaky gut opens the gate, immune dysregulation arms the troops, and inflammation leads the attack. Recognising this interplay empowers us to intervene earlier. Instead of chasing symptoms, we focus on the roots: calming nervous system tone, restoring microbial harmony, repairing the gut barrier, and re-modulating immune responses.
In our programmes, these are not abstract concepts, they become concrete pathways: the nervous system reset, nutrition and gut-microbiome plan, stress and movement practice and embodied resilience. When we treat the terrain and not just the target, we realign with health.
At Corner of Movement, we translate this science into personalized programs. Through Psychoneuroimmunology (PNI) health coaching, we guide individuals with stress-related and autoimmune conditions to regain balance through small, evidence-based lifestyle shifts.
Our Healthy Productivity corporate programs empower organizations to create environments that support the gut-brain health of their teams, reducing burnout while improving performance. And our Qi Gong sessions help activate the parasympathetic nervous system and support gut-brain alignment through movement, breath, and embodiment practices.
Your gut health is not just about digestion, it is the foundation of your body’s adaptability, your mind’s clarity, and your life’s energy.
Maria Salazar- Founder